Foreword
Foreword
With our diverse population and universal healthcare system, NHS data should be the UK’s jewel in the crown, not only to enable the highest quality of person-centred care, but also to drive research and development (R&D) and innovation to improve population health and attract inward investment. Despite this potential, the existing reality does not match the rhetoric and falls short of expectations.
Our nation boasts internationally acclaimed data assets, such as UK Biobank and the Clinical Practice Research Datalink (CPRD), which have long delivered high-quality data services to academia, government, and industry worldwide. Yet, as highlighted in the Sudlow Review ‘Uniting the UK’s Health Data’, accessing the majority of NHS data for R&D is fraught with challenges, resulting in missed opportunities for patients, the NHS, researchers, and the UK economy.
In response to the Sudlow Review's recommendation, the government has signalled an openness to establishing a health data research service. This initiative presents a crucial opportunity to transcend our current complicated and fragmented landscape to create an internationally competitive research service. This service should be grounded on the principles of user-centred design and patient engagement, genuinely addressing the needs of all stakeholders.
The task is substantial, and it is tempting to settle for optimising our existing investments, despite their known flaws. To support the government in this ambitious endeavour, we have considered three principles for the design of a national data service. Firstly, prioritising the most critical datasets for R&D to provide a strong foundation for a data service that can then be scaled and expanded. Secondly, defining the essential criteria for a sustainable health data research service, setting a clear framework for future developments. Lastly, leveraging and building on the expertise and experience of existing data services that already deliver to an international standard.
These principles have guided our evaluation of seven potential health data research service options, enabling us to offer informed recommendations for government consideration. We are poised at the threshold of potentially creating something that is not just national but truly world-leading in health data research. Our insights aim to provide a robust foundation to assist the government's decision-making, ensuring that NHS data fully realises its potential to catalyse health improvement and stimulate economic growth.
 Professor Andrew Morris CBE
Professor Andrew Morris CBEResearch UK
 Dr Richard Torbett MBE
Dr Richard Torbett MBEAssociation of the British
Pharmaceutical Industry
Purpose
What this work adds
Currently there are two published documents proposing the need for a centralised health data service supporting research uses via a National Data Trust or a National Health Data Service.
This work builds on published and unpublished discussions by:
- Distilling the minimum national datasets that should form the basis of a health data research service and can be expanded from this foundation. This approach has the greatest potential to demonstrate immediate value and avoids the danger of trying to ‘boil the ocean’ at the outset, while enabling the ambition to scale and link datasets more widely.
- Defining the essential criteria for a viable, internationally competitive and sustainable health data research service, which can serve as an evaluation tool for any data service model under consideration.
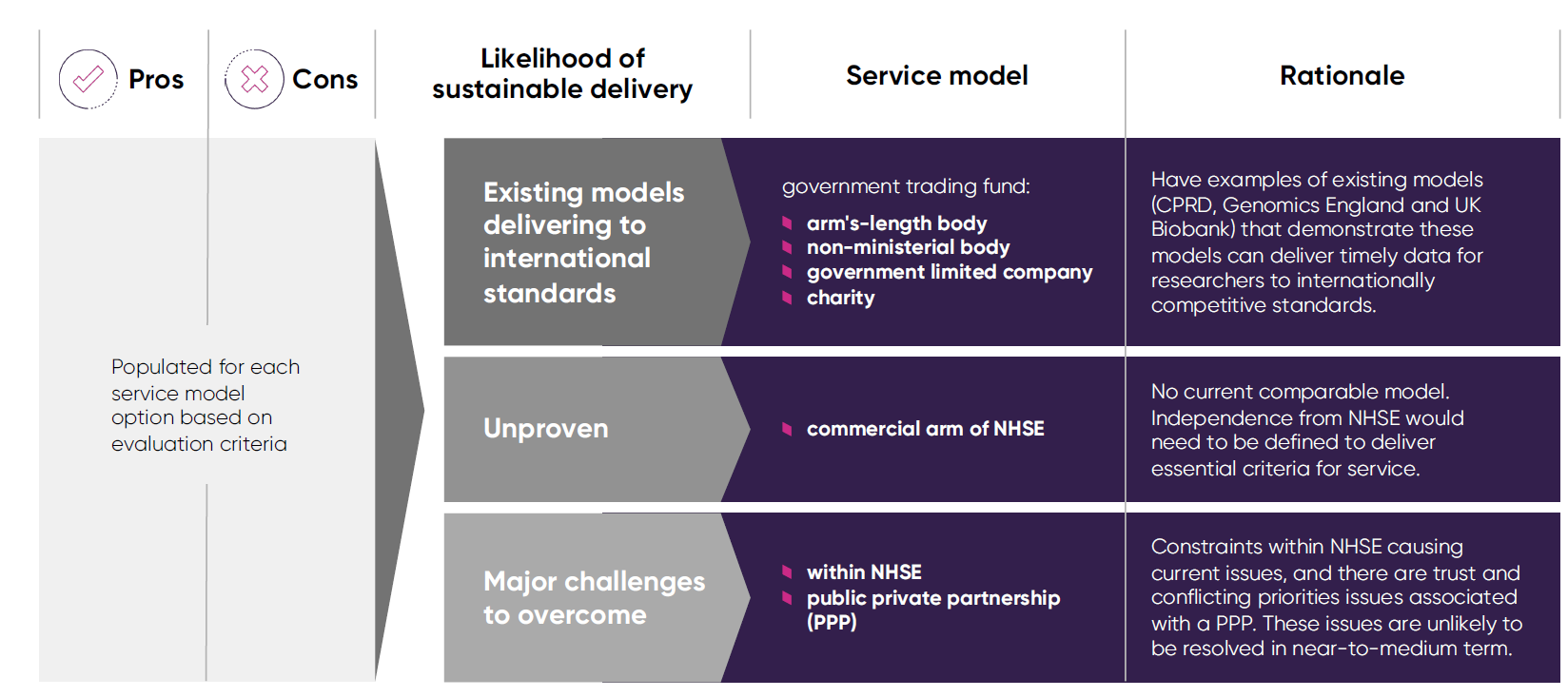
- Appraising different health data research service model options, outlining the pros and cons of each option. The aim is to demonstrate to policy makers that there are multiple options that can be explored to take this work forward, some of which are already efficiently delivering to international standards.
What this work does not seek to do
This is because:
- To the best of our knowledge, there is no model that meets all the essential criteria for a service. There are different models that are delivering internationally recognised data services and models where the challenges to overcome to achieve the ambition are substantial.
- The decision is for policy makers and our intention is to inform the debate.
2. While we drew on significant expertise and experience in the development of this work, we do not claim to represent the views of patients and the public, healthcare professionals and the full range of research data users. This is why we recommend that a wider discussion informed by this work and the work of others should take place.
Use of health data for R&D is an enabler of two government missions
Labour's five missions to rebuild Britain
“Businesses in the life sciences industry generated £108.1 billion turn over in 2021/22. There were 304,200 people employed in the UK life sciences sector in 2021/22.”
Biosciences and health technology sector statistics 2021–2022, May 2024
“A national health data service will accelerate research and analysis that benefits society.”
Sudlow Review: Uniting the UK’s Health Data: A Huge Opportunity for Society, November 2024
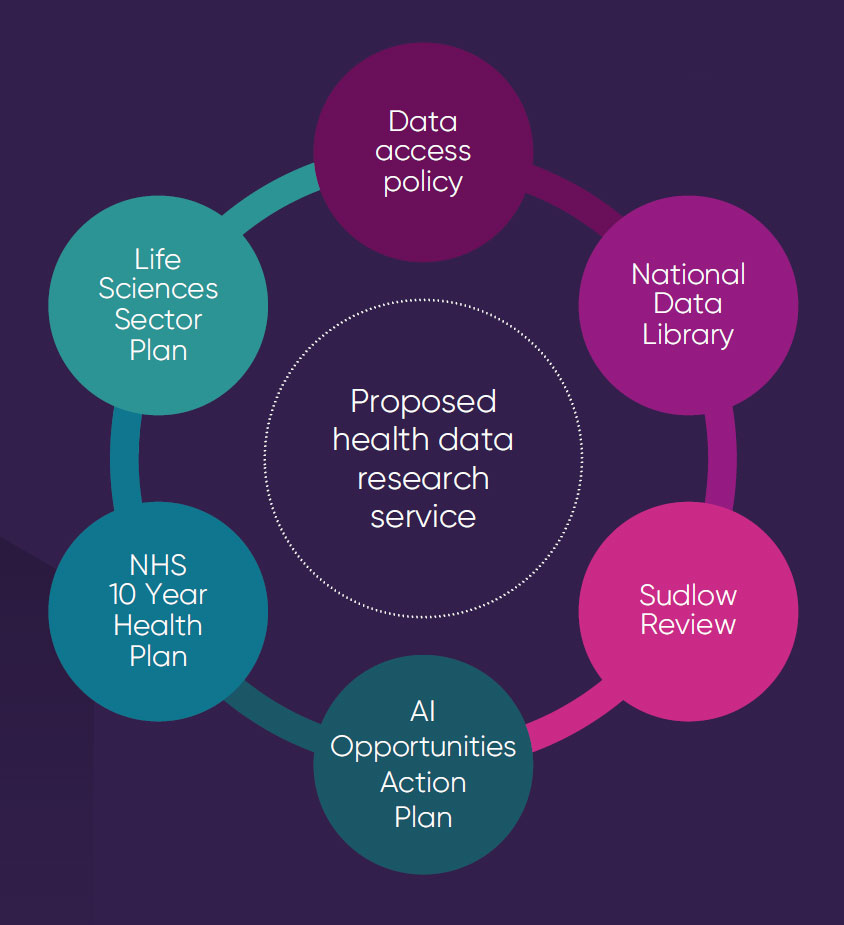
Current health data policy context in England
It is vital we seize this opportunity to ensure:
implementation plan to achieve it
Reality of the national health data research ecosystem in England
Despite the promise of NHS data being a UK unique selling point to power research and innovation, it remains largely untapped because in England there is:
of national data infrastructure
- ◆ no centralised comprehensive GP data collection
- ◆ services fragmented across NHS trusts, NHS England & MHRA (CPRD)
- ◆ variable approaches between NHSE SDE and regional SDEs
- ◆ disparity in funding mechanisms and commercial models
- ◆ each department operates in a silo,
no system-wide planning leading to
duplication, gaps and confusion - ◆ limited stakeholder engagement and
understanding of researcher data and
service requirements - ◆ pharmaceutical industry and
international regulators use CPRD
(~50% users) and few use current NHSE
services (<10% users), which have
received most recent investment
constraints
- ◆ disruption due to multiple mergers
- ◆ deprioritisation of research services
when other NHS issues arise - ◆ NHSE capacity restrictions due to
limited headcount and skills causes
long delays accessing data - ◆ NHSD/E unable to link data for CPRD
between 2021-2024, leading to major
issues for regulatory uses
Joint ABPI HDR UK project to scope options for a sustainable health data research service
Project approach to developing essential criteria and service model options
Determine priorities
and essential criteria
for a health data
research service
- consult with experts from NHS, government, charities, academia and industry
- validate which datasets should be the initial priority
- refine essential criteria for a national research service that meets needs of stakeholders and users based on expert feedback‡
Develop service
model options
- gather evidence on existing data services’ performance and delivery, financial sustainability and research user base
- in consultation with experts, identify viable service model options for a national research service
Evaluate service
model options
- consider pros and cons of each option based on essential criteria for a service
- assess service model options, drawing on evidence of existing sustainable data services and options evaluation
- propose recommendations for next steps
‡This report is the work of the ABPI and HDR UK. An expert advisory group with representatives from NHSE, DHSC, HRA, AMRC, and general practitioners were asked to comment on ABPI and HDR UK assumptions on potential service model options, essential criteria for the service, and the accuracy of pros and cons proposed for each model. The role of these organisations was advisory on these aspects of the exercise only and they were not asked to endorse this report, or any recommendations regarding the potential strategic direction for a health data research service.
What should we prioritise to maximise the value of NHS data for patients, the NHS and the economy?
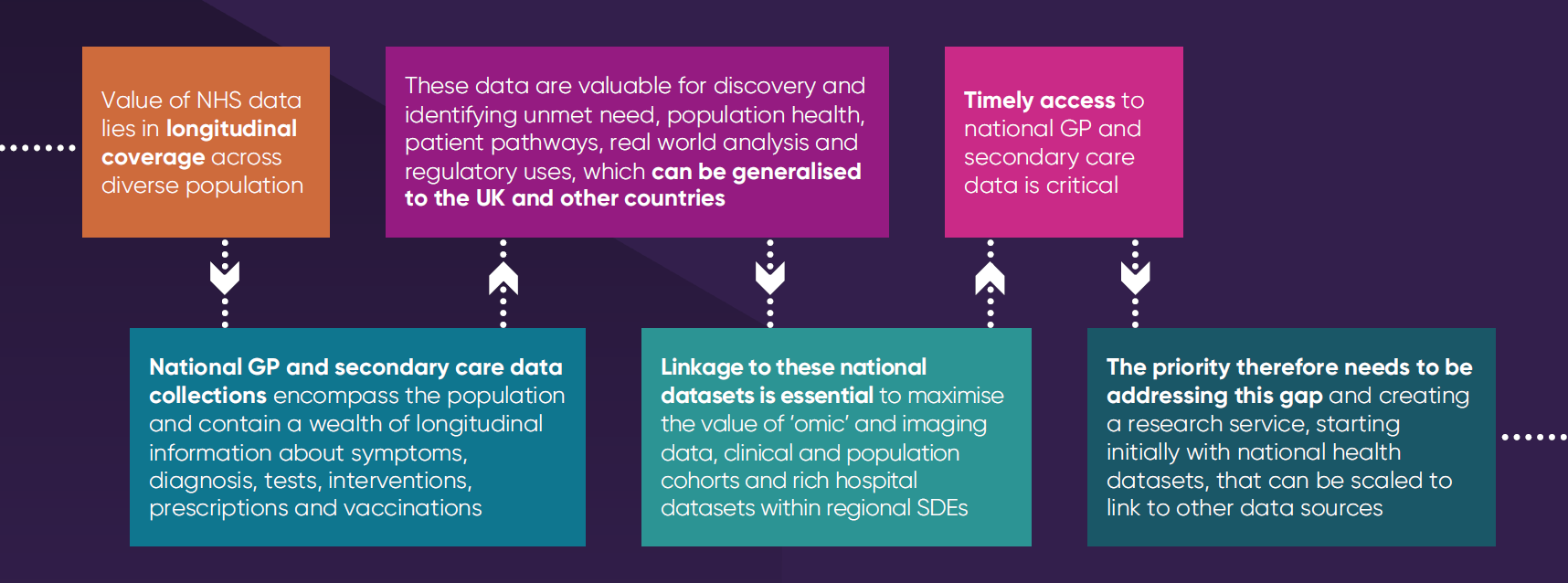
What should be the initial scope for a minimum viable national health data research service?




National datasets in England
- comprehensive GP data
- national secondary care datasets including hospital prescribing data, mortality data, audits and disease registries
Research purposes only
- access by academics, regulators, and industry researchers
- Secure Data Environment/Safe Haven by default
Research service offering
- linked data for observational research, AI and machine learning
- data linkage for participants in consented cohorts and clinical trials
Scalable
- initial focus on national health datasets
- aim to link with other UK national, regional, ‘omic’ and non-health datasets including ONS and national data library in the future
- future services to support clinical trials feasibility and recruitment
Essential criteria for a health data research service

Operate in partnership
with the NHS
- comprehensive longitudinal GP and national secondary care data collected by NHSE flows into service
- leverages operational efficiencies and reduces dependencies on GP software suppliers
Considered trustworthy by patients, the public and healthcare professionals
- Secure Data Environment/Safe Haven by default
- responsible for data controllership, with the ability to hold identifiable patient data
Deliver internationally competitive research services
- autonomy to set priorities and focus on research service delivery for all sectors
- workforce capacity and skills capability to meet user demands and support service innovation

Remove fragmentation in the research data ecosystem
- maximise government funding by combining government assets into a single fit-forpurpose service
- build on existing expertise and services that already deliver to international standards

Generate revenue to reinvest in service improvement and the NHS
- dedicated budget, ability to generate and retain income to reinvest in service expansion and the NHS
- government funding required to establish the service, with goal of achieving financial sustainability
Options for health data research service model

Evaluation criteria informed the assessment of each service model
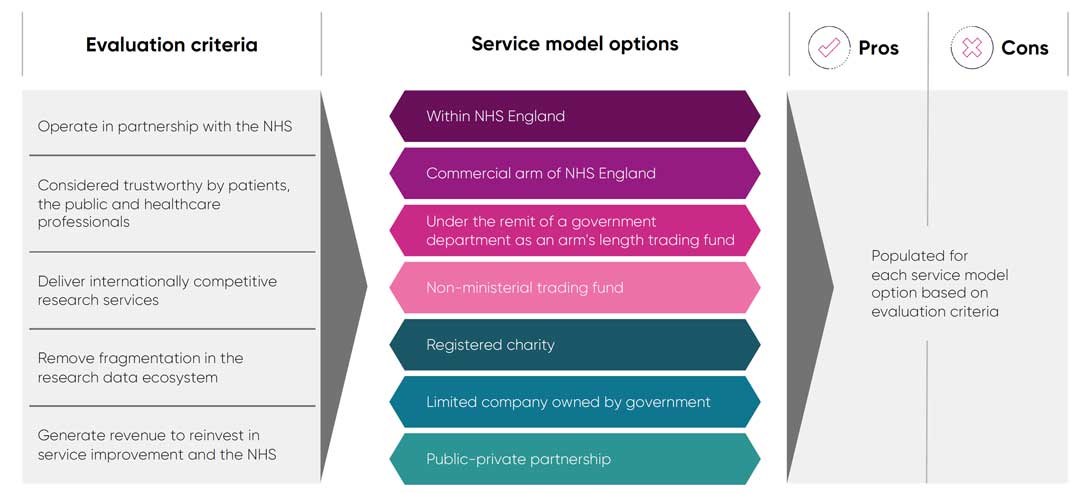
Service model option 1 - Within NHS England
Pros
- Existing remit to support secondary uses of national data collections, including issuing directions on behalf of the Secretary of State for Health and Social Care.
- Has statutory right to collect identifiable health data.
- Builds on existing infrastructure and can leverage economies of scale.
- NHSE recognised by patients and the public as having a role in collecting and using health data.
Cons
- Budget is not ring-fenced and can be/has been utilised to support frontline services.
- Current resources subject to diversion to other NHS priorities, leading to persistent issues providing timely data access for research.
- Full range of requisite specialist expertise not currently available in house. Head count restrictions prevent effective delivery of current service offerings and would not support expanded services.
- Operations constrained by annual budgets, with inability to carry forward any surplus, which creates uncertainty and hampers delivery and planning.
- Perceived risk by GPs that collection of data for secondary uses may also be used for performance management.
- Service would require creation of new senior leadership post with internal accountability akin to Chief Scientific Advisor Genomic Medicine Service role.
Service model option 2 - Commercial arm of NHSE
Pros
- Remit dedicated to research services without competing NHS delivery priorities.
- No legislative change to collect identifiable health data.
- Ability to generate income and flow surplus into continuous improvement and potentially to the NHS.
- Potential for workforce capacity flexibilities to meet service demand.
- Builds on existing infrastructure and can leverage economies of scale.
- NHSE recognised by patients and the public as having a role in collecting and using health data.
- Ability to create senior leadership post directly accountable to NHSE Executive.
Cons
- May be challenging for budget to be ring-fenced and not subject to diversion to support core NHSE or frontline services.
- Establishment of separate NHSE data body may be perceived as recreating NHS Digital, and be at heightened risk of merger back into NHSE as part of future NHS budget efficiencies.
- Salaries would follow NHS pay scales and would need to apply for exemptions for specialist roles.
- While there can be some delegated freedoms, operations may be restricted by government operational frameworks.
- Perceived risk by GPs that collection of data for secondary uses may also be used for performance management.
Service model option 3 - Government department arm’s length body trading fund
Pros
- Remit focused on research service delivery without competing priorities.
- Budget dedicated to delivering research services.
- Ability to generate income and invest surplus into expansion of services and continuous improvement.
- Flexibility to hire staff with requisite skills with potential to expand capacity to meet service demand.
- Government services generally trusted by healthcare professionals and the public.
- Ministerial support within the context of departmental responsibilities.
- Service led by senior leader.
Cons
- Overhead costs associated with supporting an independent government body, including establishing own research, IT and governance infrastructure.
- Salaries restricted to civil service pay scales and headcount may be subject to government restrictions.
- Not part of the NHS, which could affect trust by the public and healthcare professionals.
- Ability to collect identifiable data might necessitate legislative change (but might be achievable with a direction from the Secretary of State or alternative means).
Service model option 4 - Non-ministerial trading fund
Pros
- Remit focused on research service delivery without competing priorities.
- Budget dedicated to delivering research services.
- Ability to generate income and invest surplus into expansion of services and continuous improvement.
- Flexibility to hire staff with requisite skills with potential to expand capacity to meet service demand.
- Government services generally trusted by healthcare professionals and public.
- Service led by senior leader.
Cons
- Overhead costs associated with supporting an independent government body, including establishing own research, IT and governance infrastructure.
- Salaries restricted to civil service pay scales and headcount may be subject to government restrictions.
- Not part of the NHS, which could affect trust by the public and healthcare professionals.
- Ability to collect identifiable data might necessitate legislative change (but might be achievable with a direction from the Secretary of State or alternative means).
Service model option 5 - Registered charity
Pros
- Remit focused on research service delivery without competing priorities.
- Budget dedicated to delivering research services.
- Able to receive funding from third parties.
- Depending on the degree and extent of public sector control, may have flexibility to operate outside public body policies, including bringing in requisite skills at competitive pay scales, with capacity to expand to meet service demand.
- Service led by senior leader.
Cons
- Overhead costs associated with supporting an independent registered charity, including establishing own research, IT and governance infrastructure.
- Subject to Charity Commission requirements and obligations. Rules may restrict spending of any surplus.
- Depending on the degree and extent of public sector control, charity could be classified as a public body, which would limit some operational flexibilities.
- Not part of the NHS, which could affect trust by the public and healthcare professionals.
- Ability to collect identifiable data might necessitate legislative change (but might be achievable with a direction from the Secretary of State or alternative means).
Service model option 6 - Public-private partnership
Pros
- Remit focused on research service delivery without competing priorities.
- Depending on the degree and extent of public sector control, may have flexibility to operate outside public body policies, including retaining and investing surplus into expansion of services and continuous improvement, and bringing in requisite skills at competitive pay scales, with capacity to expand to meet service demand.
- Government does not have to bear the full cost and has potential to become fully financially sustainable.
- Partnership offers opportunity to have a more competitive operating model and service offering.
- Service led by senior leader.
Cons
- Overhead costs associated with supporting an independent company, including establishing own research, IT and governance infrastructure.
- Heightened risk of public and healthcare professional trust concerns due to private sector involvement.
- Pressure to achieve financially sustainability and return on investment for private sector partners could result in higher data access costs.
- Private sector investment could result in preferential data access demands and ongoing tensions between government and private investor priorities.
- Ability to collect identifiable data might necessitate legislative change (but might be achievable with a direction from the Secretary of State or alternative means).
Assessment of service models based on evaluation criteria and deliverability
Recommendations for next steps
Develop a shared vision across stakeholders
- appoint the Data for R&D programme Strategic Advisory Group, to develop a shared vision and aligned priorities for the UK health data research ecosystem
- agree realistic phased implementation plan to address greatest needs first and maximise return from government spending on health data research infrastructure
Build on services that are already delivering
- build on experience and expertise of existing research data services with a track record of delivering researcher needs to academia, regulators and industry worldwide e.g. CPRD and UK Biobank
Engage with the public,
patients and GPs
- consult with GPs, patients and members of the public to hear their views on service model options, governance, and public participation and involvement
Choose a sustainable service model
that will deliver all the essential criteria
- validate pros and cons assumptions in the options appraisal
- ensure service model chosen is scalable, sustainable and can meet all the essential criteria defined for a health data research service, including delivering services to an internationally competitive standard
Glossary
Clinical Practice Research Datalink (CPRD): A health data service providing de-identified patient data for research purposes. https://www.cprd.com/
Data access policy: Changes to how NHS data is accessed including the move from a system of data sharing to a system of data access. https://www.gov.uk/government/publications/data-access-policyupdate/ data-access-policy-update
Data Access Request Service (DARS): NHS England’s gateway to accessing NHS health and social care data. https://digital.nhs.uk/services/dataaccess- request-service-dars
Data asset: A collection of data that has value for research, such as the UK Biobank. https://www.ukbiobank.ac.uk/
Data linkage: The process of connecting different datasets for a more comprehensive analysis. https://bmjmedicine.bmj.com/content/1/1/e000087
Data (Use and Access) Bill: A proposed Government Bill with implications for health data sharing. https://bills.parliament.uk/bills/3825
Genomics England: Company wholly owned by government that analyses sequenced genomes for the NHS and provides genomic data for research. https://www.genomicsengland.co.uk/
Health data research service: A service providing secure access to health data for research and development purposes.
Longitudinal data: Data collected over a long period to track changes and trends. https://www.dundee.ac.uk/stories/data-safe-havens-uniquelongitudinal- data-drives-healthcare-innovation
National Data Library: A proposal from the Labour Party Manifesto to “bring together existing research programmes and help deliver data-driven public services. https://labour.org.uk/wpcontent/ uploads/2024/06/Labour-Party-manifesto-2024.pdf
NHS commissioning support units: Independent units that provide commissioned services back to the NHS. https://www.kingsfund.org.uk/insight-and-analysis/long-reads/whatcommissioning- and-how-it-changing
NHS England Secure Data Environment: NHS England’s Secure Data Environment platform providing access to nationally collected data sets, formerly the responsibility of NHS Digital https://digital.nhs.uk/services/secure-data-environment-service
NHS Digital (NHSD): Former national provider of data and IT systems for the NHS, now merged into NHS England. https://digital.nhs.uk/
NHS 10 Year Health Plan: Upcoming plan for how government will deliver an NHS fit for the future. https://www.england.nhs.uk/long-term-plan/
Omics data: Biological data related to genomics, proteomics, or other molecular-level information. https://rd-connect.eu/what-we-do/omics/
OpenSAFELY: NHS England commissioned software platform for analysis of electronic health records data. https://www.opensafely.org/
Public-private partnership (PPP): A collaboration between government and private companies for service delivery. https://www.independent.co.uk/voices/nhs-private-public-partnershipb2158452.html
Regional SDE: Secure data environment providing access to health data at a regional level. https://digital.nhs.uk/data-and-information/researchpowered- by-data/sde-network
Siloed data: Data stored separately without easy access across systems. https://www.computerweekly.com/news/252514852/Siloed-data-holding-back-coordinated-health-responses
Sudlow Review: An independent review highlighting the need for unified health data access in the UK. https://www.hdruk.ac.uk/helping-withhealth-data/the-sudlow-review/
Trusted research environment (TRE), also referred to as Data Safe Haven or Secure Data Environment (SDE): A secure space where sensitive data can be accessed and analysed without leaving the environment. https://understandingpatientdata.org.uk/secure-data-environments
UK Biobank: A biomedical database and research resource, established as a charity in 2006, containing data and samples from half a million UK participants. https://www.ukbiobank.ac.uk/
User-centred design: A process that focuses on what users need throughout development. https://www.experienceux.co.uk/faqs/what-is-user-centred-design/
DHSC = Department of Health and Social Care
HRA = Health Research Authority
AMRC = Association of Medical Research Charities
-
ThemeHealth Data
-
KeywordsHealth data
-
PublisherABPI, HDRUK